My Voice Matters is a national consultation series which collects the experiences people using mental health services in Ireland, and the experience of their family members, friends and carers/ supporters.
My LGBTI+ Voice Matters: A Mixed Methods Exploration of the Views and Experiences of LGBTI+ Mental Health Service Users
Drawing on the data collected as part of the My Voice Matters consultations series and in partnership with LGBT Ireland, this HSE funded project explores the views and experiences of mental health service users from the LGBTI+ community.
Key findings from the “My LGBTI+ Voice Matters” report:
- 1,127 people participated in this report
- 215 of the participants are members of the LGBTI+ community
- 43% of LGBTI+ participants reported having a poor overall experience with HSE mental health services
- 31% of LGBTI+ participants felt that they were always treated with respect and dignity by community mental health services
- 80% of LGBTI+ participants felt well-supported by their key worker to some extent at least
- Need for more LGBTI+ centered training and education for services providers
The My Voice Matters series looked at the experiences of mental health service users and their family, friends, carers and supporters. These first reports were published in March 2019.
Key findings from the Service User report:
- 1,188 people participated in this report
- 41.6% of participants indicated that they had a poor experience of HSE Mental Health Services
- 19.5% reported that they did not feel like they were treated with dignity and respect by Community Mental Health Services
- 46.0% of participants were most dissatisfied with the therapeutic supports when in inpatient mental health services.
- One in six reported having had a change of psychiatrist ‘more than four times’ in the last two years.
- Of the participants who had reported having gone to Emergency Departments to seek support for their mental health, 49.3% disagreed that they got the support they needed.
- Six in 10 participants (60.3%) reported a high focus on medication as part of their treatment and care.
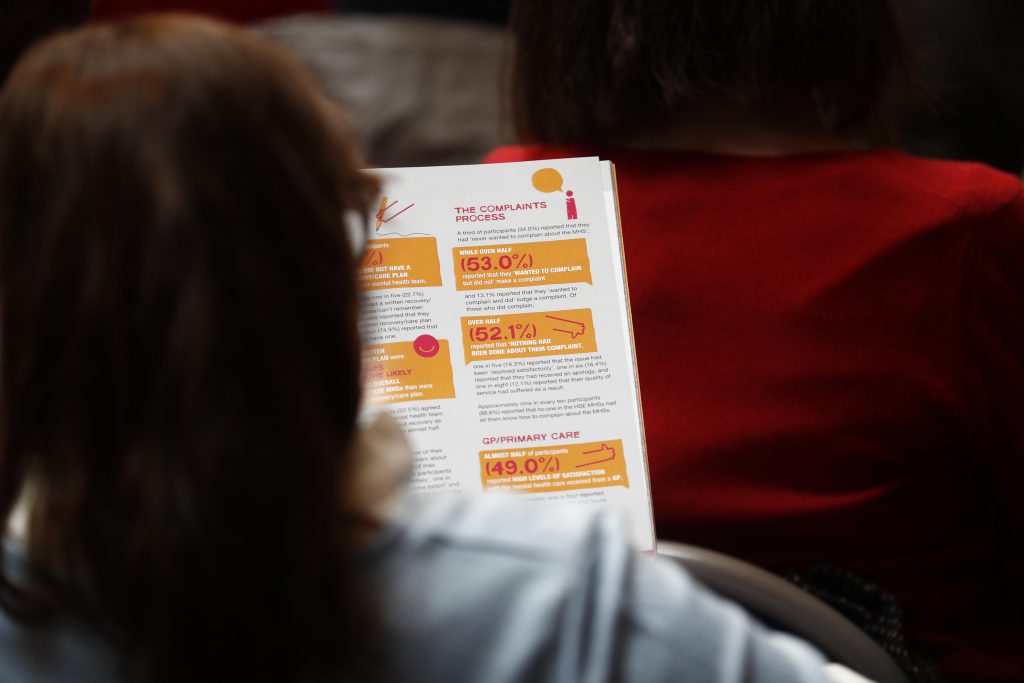
- Two-thirds of participants (66.2%) reported they did not have a written recovery/ care plan developed with their mental health team.
- Of those who did complain, 52.1% reported that ‘nothing had been done’ about their complaint.
- 49.0% reported high levels of satisfaction with the mental health care received from a GP.
Key findings from the Family Member, Friends and Carers/ Supporters report:
- 786 people participated in this report.
- 66.5% reported being dissatisfied with the information and advice they received when the person they support first came into contact with the HSE.
- 65.6% reported that they had not received information on what to do in a crisis.
- 75.9% disagreed that the HSE Mental Health Services explained how to support the person in the long term.
- Eight in 10 people (81.8%) reported they had not been let know how to make a complaint about a HSE Mental Health Service.
- One in 10 people (10.7%) agreed that they had the opportunity to provide feedback to Mental Health Services to inform service improvement.
- 71.7% of participants were dissatisfied with the extent to which the HSE Mental Health Services had considered their support needs.
- Individual counselling was the most common support access by participants, with approximately one in four (26.6%) accessing it in the last two years.
- 49.0% of participants disagreed that they ‘felt listened to by hospital staff’.
- 55.7% of participants reported low levels of satisfaction with the quality of service received by the person they support.
- Six in every 10 (60.1%) reported low levels of satisfaction that the HSE Mental Health Services had provided the individual with supports that adequately targeted their needs.
View the presentation slides from the launch which includes an overview of the My Voice Matters reports, key findings, and recommendations by clicking here.
You can read the My Voice Matters Executive Summaries and Full Reports below.
Executive Summaries:
- My Voice Matters: Mental Health Service Users – Executive Summary
- My Voice Matters: Family, Friends and Carers/ Supporters of Mental Health Service Users – Executive Summary
Photo gallery from the launch of My Voice Matters (March 2019)